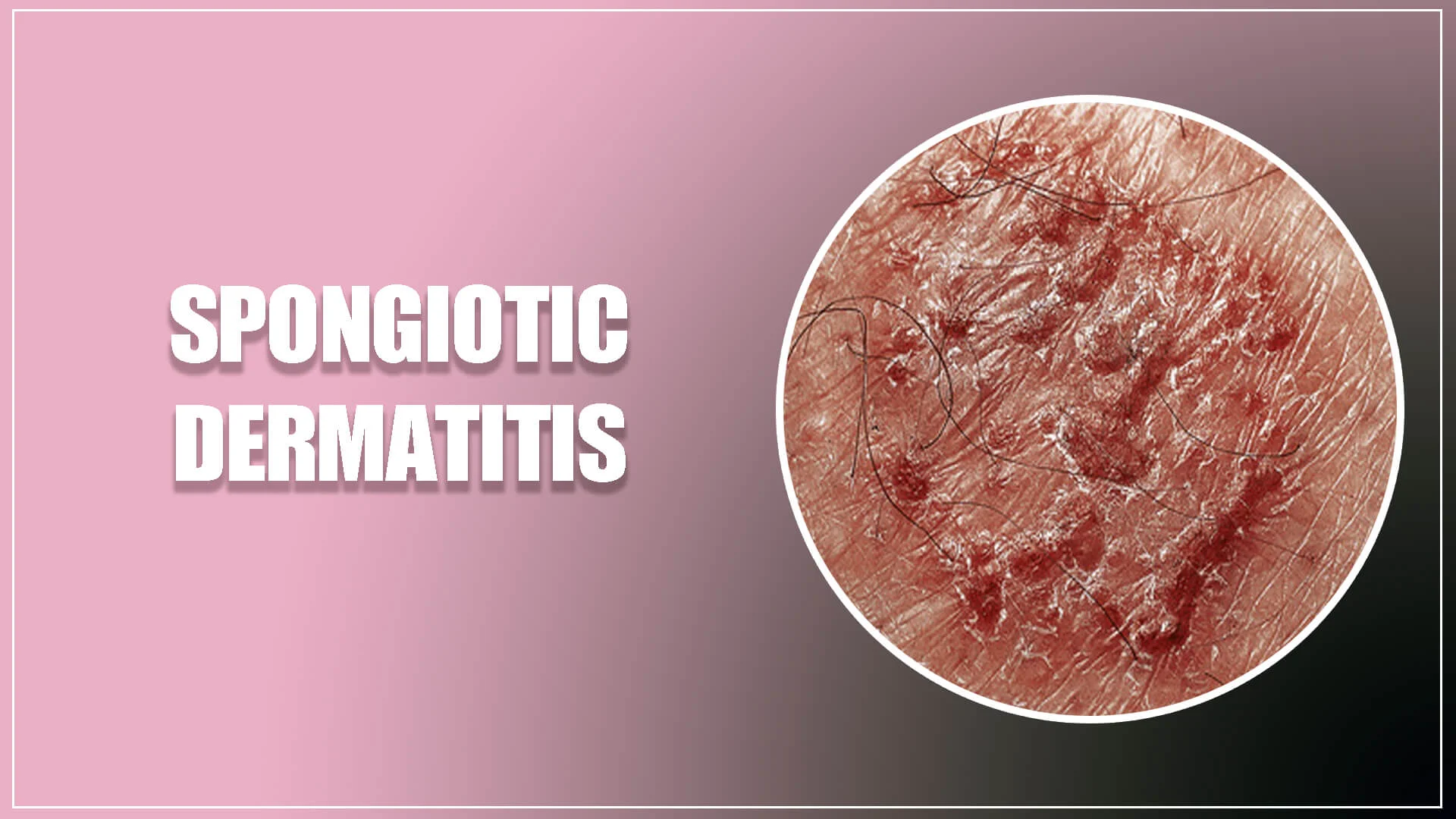
Skin that has sponge-like growths on it becomes dry, red, itchy, and cracked due to sponge-like dermatitis. Typically, there is some edema brought on by too much fluid under the skin.
Atopic dermatitis or eczema is closely related to sponge-like dermatitis. It is a common disorder that results in skin inflammation and is brought on by allergens.
The symptoms, causes, and treatments of spongiotic dermatitis will all be covered in this article’s summary.
Symptoms of Spongiotic Dermatitis
The following signs and symptoms of spongiotic dermatitis may apply to you: scaly patches of itchy skin; coin-shaped rashes; including:
- Skin blemishes
- Irritated skin
- Dandruff that is challenging to remove
- After scratching an infected area, there is leaking and infection.
- Babies with diaper rashes brought on by contact dermatitis may also develop sponge dermatitis.
Spongiotic dermatitis may occasionally be an early sign of the skin malignancy cutaneous T-cell lymphoma. Your doctor might use a skin biopsy to look for spongiotic dermatitis and other indicators of this.
What is Spongiotic dermatitis with eosinophils?
Spongiotic dermatitis: What is it? Skin that has sponge-like growths on it becomes dry, red, itchy, and cracked due to sponge-like dermatitis. Typically, there is some edema brought on by too much fluid under the skin. Atopic dermatitis or eczema is closely related to sponge-like dermatitis.

Causes of spongiotic dermatitis
Dermatitis spongiotic allergic reactions, for instance, to drugs or food. Contact with irritants such as chemicals, specific cosmetic compounds, or some metals used in jewelry. Infectious fungus stress, which can rob your immune system of its strength and lead to outbreaks.
Most common cause of spongiotic dermatitis
Most people don’t know what causes spongiotic dermatitis. The most common clinical cause of spongiotic dermatitis is atopic dermatitis. Although the exact etiology is uncertain, a mix of genetic and environmental factors appears to be responsible.
According to a recent study published in the Journal of Allergy and Clinical Immunology, those who suffer from this ailment may have a mutation in the gene that produces the protein known as filaggrin. This protein aids in keeping the skin’s outermost layer’s protective barrier in place.
Lack of filaggrin weakens the skin barrier, allowing moisture to leave and more bacteria and allergens to enter.
Along with other illnesses like asthma and hay fever, atopic dermatitis frequently runs in families.
Potential catalysts include:
- allergies, including certain foods, plants, colors, and medicines
- Irritating products include soaps, cosmetics, rubber, and some metals used in jewelry.
- elevated levels of stress
- adjustments to hormone levels
- arid or tropical climates
- heavy sweating, which can make itchy skin even worse
Psoriasiform Spongiotic Dermatitis
An inflammatory dermatosis known as psoriasiform spongiotic dermatitis develops as a result of HIV, nutritional deficits, and psoriasis. It spreads symmetrically across the scalp, torso, elbows, and knees, and superinfection results from excoriating lesions.
Chronic Spongiotic Dermatitis
Persistent spongiotic dermatitis is Chronic Skin (chronic spongiotic dermatitis) with sponge-like growths that become dry, red, itchy, and cracked due to sponge-like dermatitis. Typically, there is some edema brought on by too much fluid under the skin. Atopic dermatitis or eczema are closely related to sponge-like dermatitis.
Spongiotic Eczema
Spongiotic dermatitis is a condition that makes the skin dry, red, itchy, and cracked. It usually involves some swelling caused by excess fluid under the skin. Spongiotic dermatitis is closely associated with atopic dermatitis or eczema.
Is spongiotic dermatitis an autoimmune disease
All forms of skin inflammation are referred to as dermatitis. Atopic dermatitis and contact dermatitis are two separate forms of dermatitis. Contact dermatitis develops when a chemical or allergen comes into touch with the skin. Eczema, often known as atopic dermatitis, is an autoimmune condition. Different skin disorders can cause sponge-like dermatitis. It frequently goes hand in hand with eczema.
Spongiotic Dermatitis and Cancer
Babies with diaper rashes brought on by contact dermatitis may also develop sponge dermatitis. Spongiotic dermatitis may occasionally be an early sign of the skin cancer cutaneous T-cell lymphoma. A skin biopsy might be used by your doctor to look for spongiotic dermatitis and other indicators of this.
Spongiotic and perivascular dermatitis
It is highly common for people to have spongiotic and perivascular dermatitis, which includes a wide range of clinical disorders. Although it can occasionally be challenging to establish, a precise histological diagnosis is crucial for clinical therapy. Understanding skin microanatomy is crucial for identifying the various histological patterns of inflammatory skin disorders. Based on the compartmental microanatomy of the skin, this article discusses the non-vesiculobullous/pustular inflammatory superficial dermatoses.
Eosinophilic spongiotic dermatitis
Eosinophilic spongiotic dermatitis is characterized by the presence of intraepidermal eosinophils linked with spongiosis and is a histological trait shared by some separate inflammatory illnesses. A subjacent autoimmune bullous dermatosis, such as the pemphigus group or bullous pemphigoid, is typically seen in the early stages of isolated eosinophilic spongiosis. The primary causes of eosinophilic spongiosis are covered in this article, along with the additional research required to understand its origin.
Acral spongiotic dermatitis
The Acral spongiotic dermatitis has psoriasiform acral dermatitis, a unique clinical entity characterised by a chronic dermatitis of the terminal phalanges and substantial shortening of the affected fingers’ nail beds. The skin biopsy revealed the pathological signs of subacute spongiotic dermatitis in each case. No alterations to the bone or soft tissues were visible in the affected fingers’ X-ray results. Atopic or contact dermatitis, psoriasis, and corticosteroid-induced distal phalangeal atrophy were among the differential diagnoses for psoriasiform acral dermatitis.
Causes of spongiotic dermatitis
Eczema, atopic dermatitis, seborrheic dermatitis, and other allergic skin reactions can all exhibit sponge-like dermatitis. Spongiotic dermatitis can be brought on by allergic reactions to specific foods, drugs, or environmental factors, as well as by coming into touch with irritants such some chemicals are:
- Cosmetic compounds, or jewelry metals.
- Parasitic infection
- Stress, which might impair your defense mechanisms and result in breakouts
- Adjustments to hormone levels
- Alterations in weather or temperature
Risk factors of Spongiotic Dermatitis include:
Age. Atopic dermatitis is more common in children than adults, with 10 to 20 per cent of children and 1 to 3 per cent of adults experiencing this condition.
Allergies. A person prone to allergies is at a greater risk of developing spongiotic dermatitis.
Irritants. Prolonged contact with irritating substances, such as detergents, chemicals, or metals, can trigger the condition.
Family history. A person with a family history of atopic dermatitis is more likely to develop spongiotic dermatitis.
Spongiotic Dermatitis Diagnosis
A physician or dermatologist can determine if they have spongiotic dermatitis by looking at the patient’s skin. Additionally, they could inquire about a person’s family history, nutrition, and way of life.
A doctor may occasionally suggest a biopsy to aid in the diagnosis. During a biopsy, a small sample of skin tissue is removed and sent to a lab for analysis.
The doctor might also perform a patch test. In this test, patches containing common allergens are applied to a person’s back to examine if they result in a skin allergy.
Complications of Spongiotic Dermatitis
Scratching an itchy rash during severe flare-ups may cause dry skin to crack or blisters to flow, which can result in skin infections.
Additionally, persistent scratching can cause lichenification, a thickening of the skin. Even when the disorder is dormant, the thicker skin may always itch.
While there is no specific cure for spongiotic dermatitis, people can treat flare-ups with medications, skincare, and lifestyle changes.
Possible treatment for spongiotic dermatitis are listed below:
Daily moisturizing and washing with moisturizer rather than soap may also be beneficial.
Avoid using soaps, shower gels, and detergents because these might aggravate the skin even more.
Topical steroid creams can be used to reduce redness and irritation. Use only the recommended or suitable dosage of your medication because taking too much of it can thin your skin.
Applying topical calcineurin inhibitors to reduce inflammation during flare-ups, such as tacrolimus ointments and pimecrolimus creams. These drugs prevent a chemical from causing skin inflammation, which results in redness and irritation.
taking antihistamines to treat allergy problems. The likelihood that newer antihistamines will make you fatigued is lower.
Creams should be covered with bandages, dressings, or wet wraps to prevent rubbing off of the ointment and scratching. Children and babies shouldn’t wear wet wraps because they risk getting too cold.
Receiving phototherapy or UV light treatment. Children often shouldn’t receive this therapy. Some skin conditions may be helped by natural sunlight by lowering inflammation.
During severe or broad flare-ups, taking oral steroids, such as prednisolone, can reduce symptoms. Steroid prescriptions must be written by a physician or dermatologist.
Best moisturizer for spongiotic dermatitis
We investigate, test, evaluate, and independently suggest the top items. Articles are examined for medical correctness by medical specialists. Find out more about our procedure. We might receive a commission if you make a purchase after clicking one of our links.
The National Eczema Association estimates that over 31 million Americans suffer from some kind of eczema, a collection of skin conditions marked by a dry, itchy rash and frequent flare-ups. Lotions can be used to treat and maintain eczema even though it cannot be cured, according to Adam Smithee, MD, a board-certified dermatologist at Westlake Dermatology in Austin, Texas.
Examined and Approved
The healing ointment from Aquaphor is made with glycerin, which holds moisture. The face can be used with Eucerin’s Daily Hydration Lotion because it is non-greasy.
He advises patients to “keep a daily moisturizing regimen as dry skin is eczema-prone skin” and that lotions can help with this. “We employ topical, anti-inflammatory drugs that may help with breakthrough flares.” There are many kinds of lotions for various body parts, including the hands, body, and facial. We examined the chemicals, cost, fragrance, and usage of a large number of eczema creams. We also sought advice from professionals.